My Journey with Primary Dysmenorrhoea
I still remember the day my first period arrived, not just because it marked the beginning of a new phase in my life but because it came with a pain that would end up shaping so many of my choices, my habits, and even my prayers. I had known what menstruation was, at least the basics. My mom had told me to inform her when it happened, and Home Economics class had walked us through the steps of using pads and staying clean. Some of the girls who had started theirs spoke about it in hushed tones, giggling in groups, sometimes complaining about the inconvenience. I was expecting mine earnestly, ready to join the “big girls”.
Then, one afternoon in school, it happened. My stomach had been hurting so much that I was nauseous. When I felt a wetness I somehow knew wasn’t urine, I just knew. I hurried home. In a way, it was a surreal moment; I was crossing into womanhood, but the level of pain stopped me from revelling in it. I had heard about cramps, but nobody said they could feel like my body was being wrung from the inside. I decided to take it in stride and not make a fuss. If none of the girls at school made it a big deal, then maybe it wasn’t one. I told myself, you’ll survive it too.
By the next cycle, though, I was in severe pain. This was the kind that made me want to curl into a ball and disappear. I tried to hide it from everyone, thinking, if other girls go through theirs without complaining, why shouldn’t I? But it kept getting worse. Soon, it came with vomiting and diarrhoea. My lower back burnt, my abdomen felt like it was on fire, and I shook until tears ran down my face. This was not just cramps.
That cycle marked the beginning of a journey I never asked for and a companion I would live with for decades. I was able to put a name to what I was going through in those early years when I stumbled on a book in my mother’s library called Every Woman.
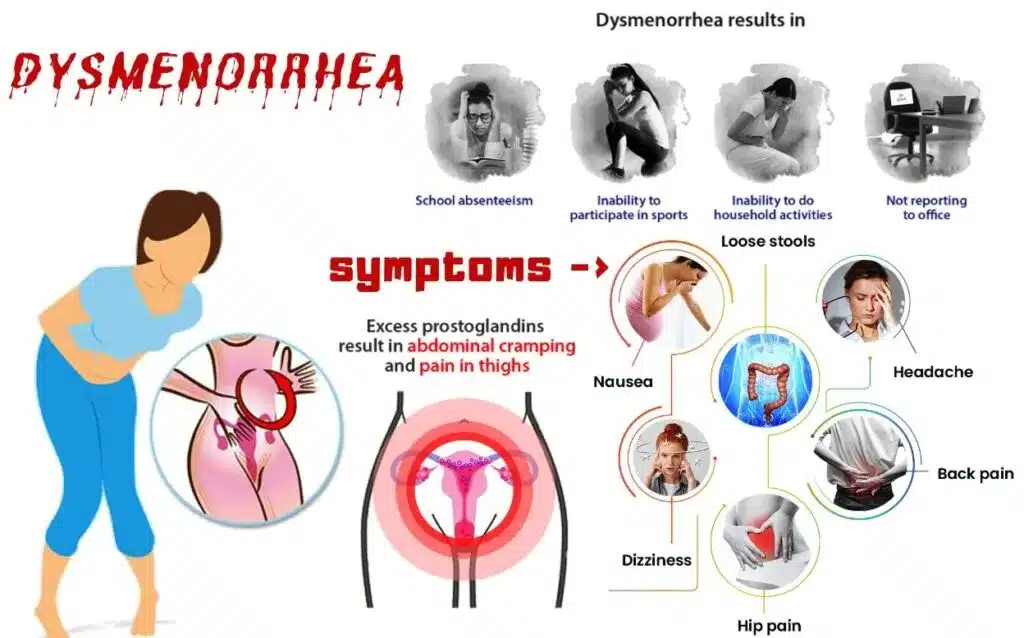
Dysmenorrhoea is the medical term for severe, painful menstrual cramps that can interfere with daily activities. Knowing its name didn’t make it go away. It just meant I had a lifelong label for what I was experiencing.
I have been in and out of hospitals over the years, asking questions, running tests, and making sure there was no underlying cause. That’s how I know for sure that what I have is primary dysmenorrhoea. I have tried different medications: prescription analgesics and hormonal contraceptives, none of which could completely stop the uterine contractions that seared through my body month after month. Painkillers hardly do anything for me; I can take the strongest over-the-counter meds and still feel the pain cut through like a hot knife. When I try to sleep through it, the contractions jolt me back to reality from wherever sleep has carried me to. In my case, I have learnt that medication doesn’t do much so I let the pain run its course, while I bear it as silently as I can.
What Living with Dysmenorrhoea Looks Like
Some symptoms are constant: the severe cramping in my lower abdomen and back, nausea, vomitting and weakness. Other symptoms vary from time to time, some months I feel pain shooting down my legs to the point I can barely walk. Other times I get headaches, diarrhoea, dizziness, or my body temperature swings from hot to cold within minutes.
I’ve had gynaecologists try to encourage me by saying that pregnancy and childbirth will be a breeze for me since I already know what contractions feel like. But that didn’t comfort me. All I could think was, “Does this mean I have years of this ahead?” I dreaded the next cycles.
Dysmenorrhoea has influenced so many decisions in my life, from the events I attend to the kind of jobs I accept. In my early years, my cycle was irregular, which made it harder to predict. I could plan to be somewhere and suddenly be forced to cancel because it came unannounced. At university, I prayed fervently that exams and tests wouldn’t fall on the first two days of my period; those days were always the worst.
Even now, if I must spend hours or days somewhere, my first thought is: “What are the bathroom facilities like? Is there water?” “Will I have my privacy?” Yeah. I don’t want to be in full view of people when I’m curled up in pain or when I’m screaming into a pillow to muffle the sound so I don’t wake the whole house.
There’s the physical pain, yes. But there’s also the emotional weight that comes with it. I rarely talk about this to anyone outside my family and a few close friends. Part of it is fear of being judged or misunderstood. The few times someone had casually said “She has cramps” in my defence, I’ve seen the sneers and heard dismissive remarks like “I have sisters and a wife, they get their periods too. What’s so special about yours?” Or “If you call in sick because of cramps, I’ll do the same next month.” These words sting. They make you swallow your pain and carry it alone.
I’ve seen women criticised for feigning pain to dodge work, so I learnt early not to bring mine up. I never write it on medical forms, never use it as an excuse for special treatment, and definitely don’t announce it in girls-only conversations at work. This is not something I brandish for pity or favours. It is simply something I live with every month. When I cannot manage it, I disappear from view until I can function again.
The pain is not the same every month. Some cycles are milder than others, though still uncomfortable. Once or twice a year, I get what I call “grace cycles”. These feature mild abdominal pain, no vomiting, no diarrhoea, and no leg pain. Those cycles feel like heaven.
Family Support
I am fortunate to have a supportive family. My mom would keep vigil with me, massaging my back, praying over me, staying up when I couldn’t sleep. My brothers would bring me hot water bottles for my abdomen and feet. My dad checked up on me too. In those moments, I felt cared for. I also prayed for my younger sisters not to experience this. And God answered. None of my sisters has this condition. That, at least, has been a relief. Neither my mom nor any family member has had this, and from what I’ve read, dysmenorrhoea is not hereditary.
Embarrassing Moments
Living with dysmenorrhoea hasn’t been without its share of embarrassing moments.
Once during a study program where I had to share a hostel room with another girl. A few weeks in, my period came, and with it, the familiar wave of severe pain. I was curled up on the tiny bed, clutching my stomach, barely able to speak. My roommate had never seen someone in that much pain before and panicked. She rushed out to call the other girls, and from where I lay, I could hear her telling them in a shaky, worried voice that she hadn’t done anything to me. I had told her it was just my period and that I would be fine, but she didn’t believe me. One of the other girls reassured everyone that she had seen something like this before, and gradually, they calmed down. I will never forget lying there in pain, and witnessing that commotion.
The second was just last year. I had gone out to catch up on errands after the first three days of my period. I was in a bus when a wave of nausea hit me so suddenly and forcefully that I barely had time to react. Before I could say a word, I was throwing up out of the window. I have never been so thankful for a window seat in my life.
Present Day
Today, dysmenorrhoea still shapes my life. There are days I can’t lift a finger, and days the pain comes and goes in intervals. Some days I can’t keep even water down, and other days I eat like I have five stomachs. It’s unpredictable, and that unpredictability is one of the hardest parts.
Working fully remote has been one of my biggest blessings. I no longer have to call in sick for two consecutive months or hide my pain at work or fear being labelled unreliable. I have more control over my time and space, and that has made a world of difference. I plan my schedule carefully to ensure no client is ever disappointed.
Why I’m Sharing This
Only about 5–15% of women experience dysmenorrhoea at the level I’m describing. The majority of women have what we consider a “normal” cycle, which still comes with discomfort but doesn’t leave them incapacitated. I am writing this not to seek pity, but to call for awareness.
We need to understand that not all menstrual pain is the same. Conditions like dysmenorrhoea, endometriosis, PCOS, and fibroids can severely affect a woman’s ability to function. Some women have had to quit work or abandon their dreams because of them. Some have lost relationships. Others power through silently, pushing their bodies to deliver results while battling pain that nobody can see.
Workplaces need to be more accommodating of invisible health conditions, not just for women, but for everyone living with internal battles, whether physical or mental. This is not me saying women should call their managers every month and take time off. This is me saying: give grace. Recognise that some people are carrying battles you cannot see. Sometimes we give more understanding to those with visible disabilities, while those with internal conditions are left to “prove” their pain.
This is me being vulnerable; opening up about something that has shaped my life for years. This is my reality, and it is also the reality of some woman out there who doesn’t talk about it, who powers through the pain, who will show up and do great work anyway.
If you are reading this and you live with dysmenorrhoea or any other invisible condition, know that you are not alone. If you are an employer, a teacher, a partner, a friend — remember that compassion goes a long way. Sometimes, all a person needs is to know that they are seen and that they are allowed to rest when they must.
For me, this pain has been my lifelong companion. I have learned to live with it, to make decisions around it, to pray through it and to survive it until the day menopause finally brings relief. Today, I am sharing it because stories like this need to be told, and because because every voice that speaks makes it a little easier for the next woman to be understood.
Stay frosty.